Pulmonary valve surgery is a medical procedure to repair or replace a damaged or diseased pulmonary valve. This valve controls blood flow from the heart's right ventricle into the pulmonary artery, which transports blood to the lungs for oxygenation.
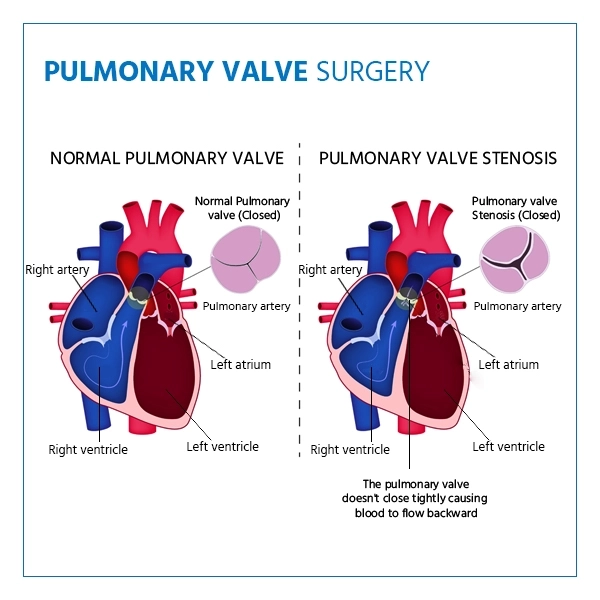
The surgery is performed to treat conditions such as pulmonary valve stenosis (narrowing of the valve) or pulmonary valve regurgitation (leakage). It helps restore proper blood flow, improve heart function, and relieve symptoms such as shortness of breath, fatigue, or chest pain.
Pulmonary valve surgery may involve:
- Valve Repair: Adjusting or reshaping the existing valve to improve its function.
- Valve Replacement: Replace the damaged valve with a biological or mechanical prosthetic valve.
This surgery can be performed through open-heart surgery or minimally invasive techniques, depending on the patient's condition and the surgeon's recommendation.
Who Needs Pulmonary Valve Surgery
Pulmonary valve surgery is performed to repair or replace a malfunctioning pulmonary valve in the heart. It is commonly required for patients with:
- Pulmonary valve stenosis (narrowing of the valve)
- Pulmonary valve regurgitation (leaky valve)
- Congenital heart defects such as Tetralogy of Fallot
- Infective endocarditis affecting the pulmonary valve
- Valve damage due to rheumatic fever
Pulmonary Valve Surgery Key Takeaways
- Type of Procedure: Surgical procedure - can involve valve repair or valve replacement with a biological or mechanical prosthetic valve. It may be performed as open-heart or minimally invasive surgery, depending on the case.
- Duration: Typically takes 3 to 5 hours, depending on the complexity of the repair or replacement.
- Anesthesia Used: General anesthesia is used throughout the procedure.
- Recovery Time: Hospital stay usually lasts 5 to 7 days. Full recovery can take 6 to 12 weeks, depending on the surgical approach and individual health condition. Cardiac rehabilitation is often recommended post-surgery.
Types of Pulmonary Valve Disease that May Require Treatment
- Pulmonary Valve Stenosis: The narrowed valve restricts blood flow to the lungs, surgery is required if symptoms deteriorate.
- Pulmonary Valve Regurgitation: The leaky valve causes blood to flow reverse directions, strains the heart, and leads to symptoms, including breathlessness.
- Tetralogy of Fallot: A congenital disability that affects the pulmonary valve, needing surgery for valve correction after other heart defects are repaired.
- Dysfunctional Bioprosthetic Valve: A worn-out biological valve needing replacement to restore heart function.
- Conduit Dysfunction: Narrowing or leakage of a previously placed conduit, often needing valve replacement.
- Endocarditis: Pulmonary valve infection requiring replacement to remove damaged tissue.
- Right Ventricular Outflow Obstruction: Blockage in the heart's outflow tract that may need surgery to fix blood flow.
Indications of Pulmonary Valve Surgery
- Pulmonary Valve Stenosis: Narrowing of the valve obstructs blood flow to the lungs, causing symptoms like fatigue and chest pain. Surgery may relieve the blockage.
- Pulmonary Valve Regurgitation: Improper valve closure leads to blood backflow into the heart, causing fatigue and shortness of breath, often requiring valve repair or replacement.
- Tetralogy of Fallot Repair: Some patients with this congenital heart defect may need pulmonary valve repair and replacement as they grow to address valve dysfunction.
- Dysfunctional Bioprosthetic Valve: Replacement may be needed if a previously implanted biological valve fails over time.
- Conduit Replacement: For patients with congenital heart defect corrections, surgery may replace narrowed or leaky conduits.
- Right Ventricular Outflow Obstruction: Blockages near the pulmonary valve might need surgical intervention to restore blood flow.
- Pulmonary Valve Endocarditis: Infection of the valve can lead to surgery to remove damaged tissue and replace the valve.
- Severe Symptoms: Surgery is considered for significant symptoms affecting quality of life or heart function.
Get a second opinion from trusted experts and makeconfident, informed decisions.
Get Second OpinionPreparing for Pulmonary Valve Surgery
Preparing for pulmonary valve repair and replacement involves thorough communication with your healthcare team, understanding the procedure, and making necessary arrangements to ensure a smooth and successful experience.
Here's how to prepare:
- Consultation: Meet your cardiologist and surgeon to review your medical history and necessary tests like echocardiograms or imaging studies.
- Medication Review: Adjust or stop certain medications, like blood thinners, as advised by your medical team.
- Quit Smoking: Stop smoking to improve healing and reduce risks.
- Stay Active: If your doctor approves, engage with light physical activity, as this may help recovery.
- Nutrition: Eat a healthy diet to boost overall health.
- Hygiene: Shower with antimicrobial soap before surgery to reduce infection risk.
- Fasting: Follow fasting instructions before surgery as advised to reduce the risk of complications from anesthesia.
Steps Involved in Pulmonary Valve Surgery
- Preoperative Evaluation: Complete tests and imaging (e.g., echocardiography) assess the heart and valve condition. Surgical options and risks are discussed.
- Anesthesia: General or local anesthesia ensures comfort during the procedure.
- Incision and Access: An incision in the chest allows access to the heart.
- Repair or Replacement: The damaged valve is repaired or replaced with a mechanical or biological valve. In some cases, a stent or conduit may be used.
- Closure and Recovery: After surgery, the incision is closed, and the heart returns to normal functioning.
- Postoperative Care: Monitoring, pain management, and wound care are provided.
- Hospital Stay and Follow-Up: Recovery begins with movement encouraged, followed by regular check-ups and possible cardiac rehabilitation.
Your health is everything - prioritize your well-being today.
Recovery after Pulmonary Valve Surgery
- Movement: Light activity is recommended to avoid potential complications such as blood clots.
- Breathing Exercises: Practice deep breathing to promote lung function and prevent congestion.
- Wound Care: Follow instructions to avoid infection and support healing.
- Medications: Take prescribed medications for pain relief, infection prevention, and heart health.
- Diet: Follow dietary recommendations for healing and heart health.
- Follow-Up: Attend appointments with your cardiologist and surgeon to monitor recovery progress.
- Gradual Activity: Resume daily activities slowly, as guided by your doctor.
- Rehabilitation: Cardiac rehabilitation can help rebuild strength and cardiovascular fitness.
- Emotional Support: Lean on your support network and seek help for emotional challenges.
- Lifestyle Changes: Adopt healthier habits like balanced nutrition, exercise, and quitting smoking.
- Patience: Recovery takes time, listen to your body and allow it to heal.