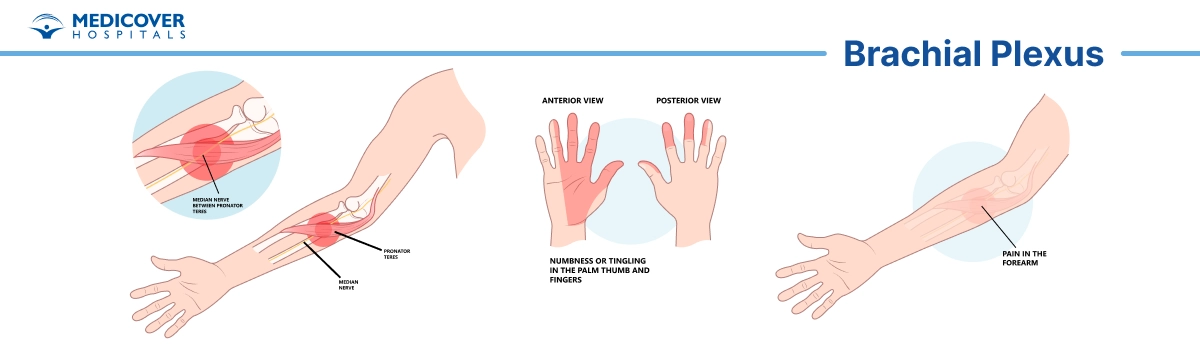
The brachial plexus is a group of nerves that starts in the neck and goes through the shoulder to the arm and hand. These nerves help you move your arm and feel sensations like touch and pain.
Sometimes, injuries from accidents, sports, or medical conditions can damage these nerves, making it hard to move your arm or hand properly.
Brachial plexus surgery is a special type of surgery that helps fix these damaged nerves. The main goal is to bring back movement and feeling in the arm and hand, helping people get back to doing everyday activities.
Different types of surgeries are used depending on the severity of the injury and the location of the nerve damage. Because the nerve network is delicate and complex, these surgeries require a great deal of skill and care.
Key Takeaways for Brachial Plexus Surgery
- Type of Procedure: Surgical (may involve nerve repair, grafting, or nerve transfer).
- Duration: Typically 3 to 8 hours, depending on the complexity.
- Anesthesia Used: General anesthesia.
- Recovery Time: Initial recovery starts in a few weeks, but full nerve healing and function restoration may take 6 months to 2 years
Types of Brachial Plexus Surgery
Brachial plexus surgery is a procedure to repair these damaged nerves. The goal is to restore movement and sensation in the affected areas. Depending on the severity of the injury, the surgery may involve:
- Nerve Grafts: Replacing the damaged nerve with a healthy nerve from another part of the body.
- Nerve Repair: Restoring function by stitching partially injured or strained nerves.
- Nerve Transfers: Connecting a healthy nerve to the damaged one to restore function.
- Muscle or Tendon Transfers: Moving muscles or tendons to improve movement in severely affected areas.
- Joint Stabilization: Correcting bone or joint issues that affect nerve function.
- Neuroma Removal: Removing abnormal nerve growths (neuromas) that cause pain or dysfunction.
- Tendon and Nerve Reconstruction: Rebuilding tendon attachments and nerve pathways to restore motor function.
- Amputation and Prosthesis: In extreme cases, amputation may be necessary, followed by the use of prosthetics.
Who Needs This Surgery?
- Patients with severe nerve injuries from accidents or sports.
- Individuals experiencing weakness, numbness, or paralysis in their arms.
- Infants with brachial plexus birth injuries (Erb's palsy).
Indications of Brachial Plexus Surgery
Brachial plexus surgery is performed to address a range of conditions and injuries affecting the brachial plexus, a complex network of nerves that control movement and sensation in the upper extremity.
The primary indications or purposes of brachial plexus surgery include:
- Traumatic Injuries: Surgery repairs damaged nerves caused by accidents or injuries to restore limb function.
- Nerve Avulsion: Reattaches or grafts torn nerve roots to regain motor and sensory functions.
- Nerve Compression: Relieves pain, weakness, or numbness caused by compression, like in thoracic outlet syndrome.
- Neuromas: Remove abnormal nerve growths to reduce pain and restore function.
- Loss of Function: Restores movement through nerve, tendon, or muscle transfers.
- Chronic Pain: Surgery alleviates persistent pain from nerve damage or injuries.
- Recurrent Palsy: Addresses ongoing weakness or deformities in conditions like obstetric brachial plexus palsy.
- Tumors: Removes growths, compressing brachial plexus nerves to restore function.
- Failed Non-Surgical Treatments: Surgery is considered when physical therapy or medications don't help.
- Functional Improvement: Enhances nerve pathways and coordination for better outcomes.
Get a second opinion from trusted experts and makeconfident, informed decisions.
Get Second OpinionBenefits of Brachial Plexus Surgery
Brachial plexus surgery offers several potential benefits, including:
- Restoration of Function: Improves limb functionality by assisting in the recovery of sensory and motor control in the injured arm.
- Pain Relief: Reduces or eliminates chronic pain caused by nerve damage.
- Improved Quality of Life: Enhances daily living by improving mobility and reducing disability.
- Muscle Strength Recovery: Allows recovery of muscle strength and coordination in the injured limb.
- Nerve Regeneration: Encourages nerve repair and regeneration, particularly with nerve grafts or transfers.
- Restored Independence: Supports improved ability to perform daily tasks and activities, reducing dependence on others.
Preparation for Brachial Plexus Surgery
Preparing for brachial plexus surgery involves careful planning, communication with your medical team, and making necessary arrangements to ensure a successful surgical experience and smooth recovery.
Here are steps you can take to prepare for brachial plexus surgery:
- Consultation: Arrange a consultation to go over your medical history, the procedure, and the dangers. As advised, undergo preoperative testing.
- Choose a Surgical Team: Research experienced surgeons and consider a second opinion to understand your condition fully.
- Informed Consent: Discuss treatment options and sign consent after understanding the risks and benefits.
- Preoperative Instructions: Follow fasting and medication instructions. Consider quitting smoking to help with healing.
- Arrange Transportation and Support: Plan for someone to drive you to and from the hospital and assist with post-surgery care.
- Health Optimization: To maximize recovery, manage long-term illnesses, and lead a healthy lifestyle.
- Home Preparation: Make sure your house is comfortable and has easy access to necessities while you're recovering.
- Emotional Preparation: Practice relaxation techniques to manage anxiety and seek emotional support.
Procedure Steps for Brachial Plexus Surgery
During a brachial plexus surgery, the specific procedures performed will depend on the nature and severity of the injury or condition affecting the brachial plexus. The surgical approach may involve nerve repair, nerve grafting, nerve transfers, muscle transfers, tendon transfers, and other techniques.
Here is an overview of what may happen during brachial plexus surgery:
- Anesthesia: To guarantee your comfort and pain management throughout the treatment, you will be given either general or regional anesthesia.
- Incision: The surgeon cuts the affected area, depending on the size of the surgery.
- Nerve Assessment: The surgeon evaluates nerve damage and uses mapping techniques to locate functional nerves.
- Nerve Repair or Grafting: Damaged nerves may be sutured or grafted with healthy tissue to restore function.
- Nerve Transfers: If nerves are severely damaged, nearby healthy nerves are redirected to restore function.
- Muscle/Tendon Transfers: If muscles or tendons are affected, they may be moved or redirected to restore movement.
- Reconstruction: Corrective procedures may be done if bone or joint issues are contributing to nerve problems.
- Closure: The incision is closed with sutures or staples, and dressings are applied.
Your health is everything - prioritize your well-being today.
Who Will Perform Brachial Plexus Surgery?
Brachial plexus surgery requires a specialized team of healthcare professionals:
- Neurosurgeons
- Orthopedic Surgeon
- Plastic Surgeon
- Hand Surgeon
- Anesthesiologists
- Physical Therapist
- Occupational Therapist
- Rehabilitation Specialist
Complications of Brachial Plexus Surgery
Brachial plexus surgery is a complex nerve repair procedure and, like all surgeries, comes with potential risks and complications.
These may include:
- Infection at the surgical site
- Bleeding or hematoma formation
- Nerve damage or worsening of existing nerve function
- Chronic pain or increased sensitivity in the operated area
- Failure of nerve grafts or transfers to restore adequate function
- Limited or incomplete recovery of muscle strength or movement
- Scar tissue formation that may compress nerves or reduce mobility
- Stiffness or reduced range of motion in the shoulder, arm, or hand
- Anesthesia-related risks, such as allergic reactions or breathing issues
Recovery outcomes depend on the severity of the nerve injury, the type of surgery performed, and the patient's age and overall health.
Recovery after Brachial Plexus Surgery
Recovery after brachial plexus surgery is a gradual process that involves careful postoperative care, rehabilitation, and patience.
Here's what you can generally expect during the recovery period:
- Hospital Stay: Depending on the complexity of the procedure, you should anticipate a length of stay in the hospital for monitoring following surgery.
- Pain Management: Medication and strategies will be used to relieve pain.
- Wound Care: To avoid infection and guarantee appropriate healing, according to the care guidelines.
- Rehabilitation & Therapy: Movement and circulation are the main focus of physical therapy's first phase. Strength and coordination will gradually improve with exercise.
- Nerve Re-Education: Certain workouts can assist in stimulating muscle activation and retraining nerves.
- Splinting & Bracing: Braces or splints may be applied to support the limb while it heals.
- Long-Term Recovery: Physical therapy may last several months. Strength and function will gradually improve over time.
- Follow-Up: Routine examinations are required to track recovery and modify treatment as needed.
Lifestyle Changes After Brachial Plexus Surgery
After brachial plexus surgery, making certain lifestyle changes can help support your recovery, enhance the healing process, and improve the long-term outcomes of the surgery.
Here are some lifestyle changes and considerations to keep in mind:
- Follow Medical Instructions: Meet to discuss wound care medications and attend follow-up appointments.
- Physical Therapy: Engage fully in therapy to regain strength and mobility.
- Nutrition & Hydration: Eat a nutritious diet and drink plenty of water to support healing.
- Quit Smoking: Smoking can slow recovery and nerve regeneration.
- Rest & Sleep: Prioritize quality sleep to aid tissue repair.
- Stress Management: Use relaxation techniques to reduce stress and promote healing.
- Avoid Overexertion: Follow activity guidelines and avoid strain.
- Good Posture: Maintain proper posture to protect healing areas.
- Patience: Stay patient with the recovery process and focus on self-care.
- Open Communication: Inform your healthcare team of any concerns or changes.