Calcified lesions, or calcifications, refer to the buildup of calcium deposits in tissues or organs within the body. These deposits can occur in various areas and may be visible in imaging studies such as X-rays, CT scans, and MRIs.
Calcified lesions can arise for different reasons and vary in size, shape, and composition. They often warrant further investigation and medical attention to determine their underlying cause and potential health implications.

Key Takeaways of Calcified Lesions
- Type of Procedure: Non-surgical, minimally invasive, or surgical (based on location)
- Duration: 30 mins - 2 hours
- Anesthesia Used: Local or general
- Recovery Time: Few days to 6 weeks, depending on procedure type
Types of Calcified Lesions
There are several types of calcified lesions, each with its own characteristics:
Atherosclerotic Calcifications
- Occur in blood vessel walls due to plaque buildup from atherosclerosis
- Can lead to narrowed or hardened arteries, increasing the risk of heart attack or stroke
Soft Tissue Calcifications
- Found in tendons, ligaments, or muscles
- Often result from injury, chronic inflammation, or degenerative conditions
- May cause pain, swelling, or limited mobility
Visceral Organ Calcifications
- Occur in organs like the kidneys, liver, or lungs
- Often linked to chronic infections, inflammation, or metabolic disorders
- Examples include renal stones, lung granulomas, or hepatic calcifications
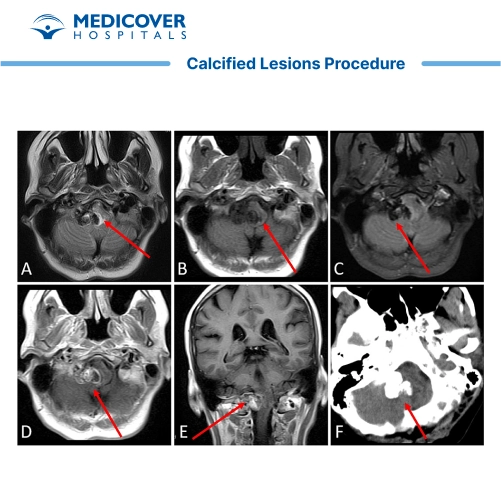
Brain Calcifications
- Can be caused by congenital infections (e.g., TORCH), metabolic disorders, or neurodegenerative diseases
- May present with seizures, cognitive impairment, or other neurological symptoms
Dystrophic Calcifications
- Occur in damaged or necrotic tissues
- Commonly follows trauma, surgery, or localized inflammation
- Calcium levels in the body are usually normal
Metastatic Calcifications
- Arise due to calcium-phosphate imbalance in the bloodstream
- Often seen in hypercalcemia, chronic kidney disease, or hyperparathyroidism
- Deposits form in otherwise healthy tissues
Clinical Indications of Calcified Lesions Surgery
Calcified lesions may signal the presence of underlying diseases or pathological changes, depending on their location:
- Atherosclerotic Calcifications: Indicate advanced vascular disease, may lead to angina or ischemia
- Soft Tissue Calcifications: Suggest chronic inflammation, trauma, or degenerative disease; often cause pain and reduced motion
- Visceral Organ Calcifications: May indicate chronic infection, renal stones, or organ damage
- Brain Calcifications: Linked to congenital infections, metabolic disorders, or neurodegeneration
- Dystrophic Calcifications: Indicate localized tissue injury in the setting of normal calcium levels
- Metastatic Calcifications: Reflect systemic metabolic disturbances such as renal failure or endocrine imbalances
Get a second opinion from trusted experts and makeconfident, informed decisions.
Get Second OpinionPreparing For the Calcified Lesions Procedure
- Gather Medical Information: Collect your medical history, including past diagnoses, medications, surgeries, and family health history to help your doctor understand your overall health.
- List Symptoms and Concerns: Note down any symptoms you're experiencing and any questions or concerns about the calcified lesion for your appointments.
- Research Healthcare Providers: If you haven't been referred to a specialist, research doctors specializing in areas like orthopaedics, cardiology, or dermatology for treatment of calcified lesions.
- Schedule Appointments: Make appointments with healthcare providers and ask your primary care doctor for referrals if needed.
- Write Down Questions: Prepare a list of questions to ask your doctor about the lesion, its causes, treatment options, and expected outcomes.
- Prepare Relevant Documents: Bring your medical records, test results, and imaging studies (like X-rays or MRIs) to your appointments for better assessment.
- Review Your Medications: List all the medications, supplements, and vitamins you're taking and share them with your doctor for a complete medical overview.
- Prepare for Diagnostic Tests: If tests like blood tests or imaging studies are needed, follow the instructions given by your healthcare provider, such as fasting or wearing suitable clothing.
- Ask About Treatment Options: Discuss treatment options with your doctor, including the risks, benefits, and expected results.
Procedure For Calcified Lesions Surgery
The management and treatment approach for calcified lesions depends on the underlying cause, the location of the calcifications, and the potential impact on the individual's health. Here are some common approaches used for calcified lesions:
- Diagnostic Assessment: If calcified lesions are found, further tests, including blood tests, biopsies or imaging, might be done to determine their cause and nature.
- Observation and Monitoring: For small, asymptomatic calcifications, physicians may also monitor over time with routine imaging to look for change.
- Lifestyle Changes: Making changes in your lifestyle like improving heart health and eliminating risk factors like high blood pressure and cholesterol can help with the management of certain types of calcifications.
- Medications: We can use medications to relieve symptoms, reduce inflammation, and prevent further calcifications, depending on the etiology.
- Physical Therapy and Rehabilitation: If calcifications affect soft tissues or joints, physical therapy can improve mobility, relieve pain, and prevent complications.
- Surgical Removal: Surgery may be needed if the calcifications cause discomfort or impair organ function, especially in more severe cases.
- Treatment of Underlying Conditions: Addressing the underlying cause, like an infection or inflammation, can help prevent further calcification.
- Medications to Manage Calcium Levels: For metastatic calcifications, medications can help regulate calcium and phosphate levels to prevent further deposition in tissues.
Your health is everything - prioritize your well-being today.
Specialist Performing the Calcified Lesions Procedure
Calcified lesions are generally managed by the following specialists based on the location and etiology of the lesions:
- Radiologist: To diagnose and monitor calcified lesions using imaging studies, including X-rays, CT scans, or MRIs.
- Cardiologist: If the calcifications are associated with atherosclerosis or heart disease, that condition will be managed by a cardiologist.
- Orthopedic Specialist: You've likely heard of an orthopedic doctor if calcified lesions are present in bones or joints, and this doctor would formulate a treatment plan, including any necessary surgery or rehabilitation.
- Rheumatologist: If the calcifications are associated with autoimmune or inflammatory conditions, the rheumatologist assists with management of the underlying cause.
- Oncologist: If the calcifications are related to cancer or metastatic conditions, an oncologist might be required for treatment.
- Surgeon: The calcified lesions may need to be surgically removed by either a general surgeon or a specialized surgeon, depending on the location.
- Nephrologist: If the calcifications are in the kidneys, a nephrologist will treat the condition.
The relevant specialist will be determined based on the specific location, cause, and health implications of the calcified lesions.
Recovery After Calcified Lesions
The recovery process after treatment for calcified lesions can vary depending on factors such as the location of the lesion, the underlying condition, and the type of treatment received. Here are some general considerations for recovery:
- Follow Medical Recommendations: Following your healthcare provider's post-treatment instructions is crucial. This might include wound care, medication schedules, and activity restrictions.
- Rest and Recovery: Depending on the treatment, you may need to rest and limit physical activity. Give your body the time it needs to heal.
- Pain Management: If you experience pain or discomfort after treatment, your healthcare provider may prescribe pain medications or recommend over-the-counter options.
- Wound Care: If your treatment involves an incision or wound, follow your healthcare provider's instructions for cleaning and dressing the wound to prevent infection and promote healing.
- Physical Therapy: In cases where the lesion affected mobility or function, your healthcare provider may recommend physical therapy to help restore strength, flexibility, and functionality.
- Rehabilitation Exercises: Depending on the location of the lesion and the type of treatment, you might be prescribed rehabilitation exercises to regain strength and mobility.
- Follow-Up Appointments: Attend all scheduled follow-up appointments with your healthcare provider. These appointments allow them to monitor your progress, assess healing, and address concerns.
- Manage Symptoms: If you experience new or worsening symptoms after treatment, contact your healthcare provider promptly. They can help determine whether it's a normal part of recovery or requires further attention.
- Gradual Return to Normal Activities: As you recover, gradually reintroduce activities into your routine as your healthcare provider advises. Avoid overexertion and listen to your body.